Often sustained during difficult deliveries, brachial plexus injuries can lead to long-term impairments and disability. But many traumatic births – along with severe cases of nerve damage – are perfectly avoidable.
- Over four decades of proven legal experience.
- Our lawyers have secured millions in compensation.
- Call us today for a free consultation at no obligation.
We believe that every child deserves a voice. Our experienced malpractice attorneys can help.
Severe childbirth injuries are shockingly common, but every child – and every family – deserves to be treated individually.
"Brilliant!" They kept me in the loop all the way through to settlement. Good people!
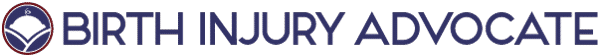
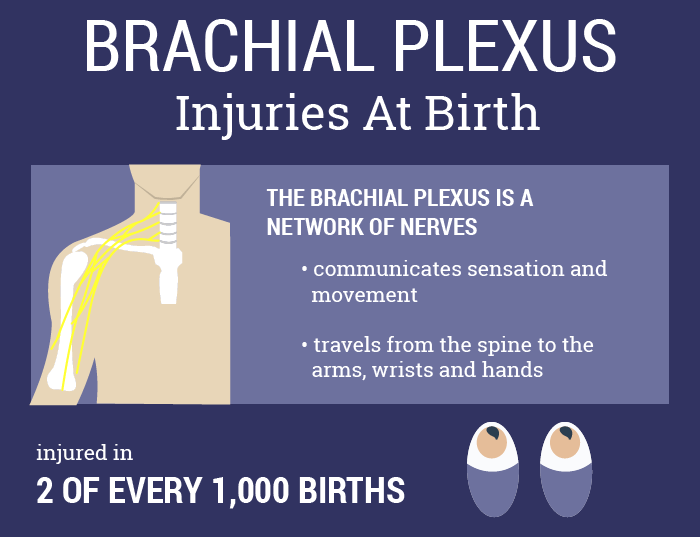
During traumatic deliveries, some infants suffer injuries to the brachial plexus, a bundle of nerves that transmits electrical signals between the spine and the shoulder, arm and hand. Brachial plexus injuries can cause paralysis or weakness – sometimes permanent disability – in the affected limb.
What Is Brachial Plexus Injury?
Most babies suffer brachial plexus injuries during the delivery process, often as a result of obstetric intervention. When an infant becomes stuck in the birth canal, some obstetricians attempt to manually reposition the child’s body. In some cases, these maneuvers involve pulling on an infant’s arms, shoulder or head. Although reasonable amounts of force can stretch the brachial plexus nerves, excessive force can injure the nerves severely.
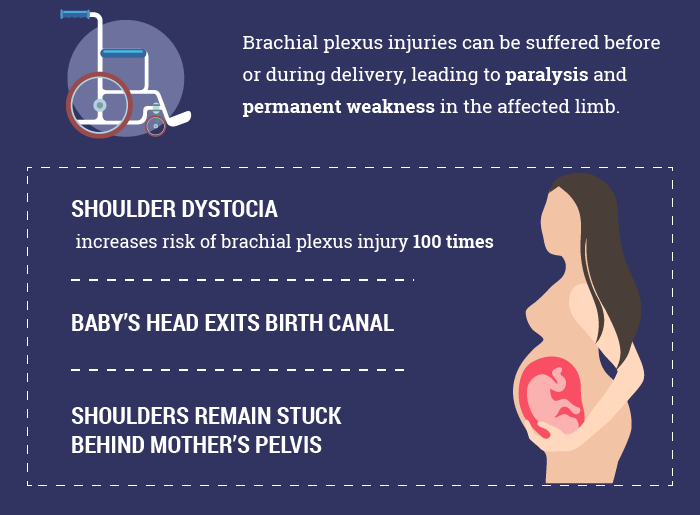
Minor injuries usually result in arm weakness or paralysis, but these symptoms often subside several days or weeks after a child’s birth. Thankfully, nearly half of all children who sustain brachial plexus injuries during childbirth will heal naturally over time. Most won’t require any medical treatment at all, although some families will be burdened by costly physical therapy regimens. Other children, on the other hand, will be left with life-long disabilities, including severe “palsy” disorders, like:
- Erb’s Palsy
- Klumpke’s Palsy
Severe injuries can lead to permanent paralysis and a total loss of feeling in the affected limb.
Nerve Injuries: Stretch, Rupture Or Tear
On a fundamental level, there are three major ways a nerve can be injured:
- Neurapraxia – when a nerve is stretched inside the spinal cord, but does not break entirely. Neurapraxia is the most common form of nerve injury, and also the least severe. In children, neurapraxia-type brachial plexus injuries generally heal on their own after several months.
- Rupture – when a nerve is stretched to the point of breaking. Rupture-type injuries don’t usually heal of their own accord, and medical intervention is likely.
- Avulsion – when a nerve is torn from the spinal cord itself. Avulsions are the most serious type of nerve injury. In many cases, avulsions cannot be repaired surgically, although surgeons have found some success with nerve grafts.
While neurapraxia-type injuries generally heal naturally, a secondary complication can make surgery necessary. As injured nerves heal, they begin to produce scar tissue. Excessive scar tissue pinches the nerve, which can lead to pain, and impairs its ability to transmit electrical impulses. Intervention may be required to remove this scar tissue, and reconnect the nerve to the muscles it controls.
Types Of Brachial Plexus Injuries
The long-term consequences of brachial plexus trauma depend both on which nerves have been injured and how severely those nerves have been damaged, according to Johns Hopkins Medicine. Brachial plexus injuries are often referred to as brachial plexus palsies, since they result in at least some degree of paralysis.
As a group of nerves, the brachial plexus allow for movement and sensation in the shoulder, arm, elbow, wrist and hand. Each nerve fiber begins in a different vertebrae of the spine, and researchers define two basic groups of these nerves.
The two nerves that begin in vertebrae C5 and C6, higher up on the neck, are referred to as the upper brachial plexus. Nerves in the upper brachial plexus control movement in the shoulder, bicep and elbow. Under those two nerves lie three other nerves, originating in vertebrae C7, C8 and T1, which doctors call the lower brachial plexus. The lower brachial plexus nerves control movement in the wrist, hand and fingers.
Erb’s Palsy
Most children who sustain brachial plexus injuries will have the upper brachial plexus nerves injured. On the affected side, a child may be unable to move the shoulder, but can retain control over the fingers. The resulting condition is often called Erb’s palsy after the German doctor who first identified the injury.
Many researchers limit the definition of Erb’s palsy to injuries in which the C5 and C6 nerves have been entirely severed, rather than stretched or minimally torn.
Complications & Long-Term Effects
Loss of sensation and movement in the affected arm are the most common, and most direct, effects of Erb’s palsy. Many of the arm’s muscles, however, are likely to atrophy without frequent physical therapy, which can lead to further impairments in motion and muscle control.
Sustained at an early age, brachial plexus injuries can affect the development of a child’s arm. While the neurological and muscular impairments are most pronounced, an infant’s cardiovascular system can also be affected. In some cases, the vessels that supply the affected arm with blood fail to develop properly, leading to problems with temperature regulation and wound healing.
Erb’s palsy need not be permanent. In minor cases of the disorder, children may experience only partial paralysis that resolves over the course of several months. Healing can occur on its own, although many children require the intervention of medical specialists to improve muscle control.
Klumpke’s Palsy
Klumpke’s palsy involves some level of injury to the lowest nerves of the brachial plexus, those starting in the C8 and T1 vertebrae. Children can be left with impairments in the wrist, hand and fingers.
In Horner’s syndrome, an associated condition caused by more severe injuries to the T1 nerve and a set of facial nerves, children will present additional symptoms. Beyond hand and wrist impairments, people with Horner’s syndrome generally have a drooping eyelid and permanently constricted pupil on the affected side.
Symptoms Of Brachial Plexus Injury In Infants
Because the signs and symptoms of a brachial plexus injury can vary, doctors often diagnose the condition by comparing one arm’s capabilities to those of the other arm. Significant differences in range of motion and gripping abilities can be a sign that nerve damage has occurred. Other potential symptoms include:
- Abnormal arm, wrist or hand positions. In cases of Erb’s palsy, the arm is often turned inwards and held close to the body.
- Continually bent elbow
- Weakness or limpness in the arm
- Difficulty moving the arm without assistance
- Difficulty controlling the movement of the arm
An infant’s reflex responses may also be affected by a brachial plexus injury. Impairments in the Moro reflex are particularly common. In their first months of life, most children respond automatically to sensations of falling. The Moro reflex is a natural reaction, initiated by a sudden loss of support, in which the child’s arms spread outwards and then close tight to the chest again. In babies with a brachial plexus injury, this reflex is usually impaired, if not entirely absent.
Brachial Plexus Injury Causes: Shoulder Dystocia
Brachial plexus injuries are particularly common in cases of shoulder dystocia.
Shoulder dystocia is a delivery complication in which a child’s head emerges from the birth canal, but their shoulders become lodged behind the mother’s pelvis. To prevent further complications, including fetal oxygen deprivation, obstetricians almost always intervene manually, using their hands to encourage an infant’s body through the birth canal.
While gentle pressure is often a necessary, albeit undesirable, requirement under the circumstances, doctors must use every reasonable caution to prevent injury to the infant.
Managing Shoulder Dystocia
Simple physical observations should be enough to diagnose shoulder dystocia. Many doctors refer to the condition’s classic symptoms as the “turtle sign.” The infant’s head will emerge from the vagina, and then pull back towards the birth canal, a sudden movement that often causes the child’s cheeks to puff out. To the eyes of some, this sequence of events looks a lot like a turtle sticking out its head then returning to the safety of its shell.
Once shoulder dystocia is recognized, however, the complication becomes a medical emergency. Of particular importance is ensuring that the child is delivered before the umbilical cord becomes pinched shut, cutting off the child’s oxygen supply. But since obstetric intervention can itself be a cause of harm, including brachial plexus injuries, doctors must use extreme care to ensure that unnecessary injuries are prevented.
HELPERR
Obstetricians have even developed a mnemonic device that outlines potential solutions in the case of shoulder dystocia, HELPERR:
- H – Call For Help
Most hospitals have a prearranged plan in place when shoulder dystocia or another delivery complication occurs. Necessary equipment and personnel should be called to the birth suite. In most cases, an anesthesiologist and specialist in neonatal resuscitation are usually requested at this time.
- E – Evaluate For Episiotomy
An episiotomy is a surgical incision in the area of muscle between the anus and the vagina, intended to widen the vaginal opening and increase the passageway for an infant’s delivery. Episiotomy is not actually required in many cases of shoulder dystocia, since the shoulders have become stuck behind the pelvic bone, not the muscular region of the perineum. Obstetricians, though, are often instructed to evaluate the situation on a case-by-case basis. Episiotomy can be indicated if an obstetrician requires more room to perform manual repositioning maneuvers.
- L – Legs
Most obstetricians agree that the McRoberts maneuver is an appropriate first step in dealing with shoulder dystocia. In the McRoberts maneuver, the mother is instructed to bring her knees to her chest (often “knees to nipples” is the exact instruction), to simulate a squatting position. This can increase the pelvic inlet and remove obstructions to the child’s delivery. The McRoberts maneuver alone is believed to resolve up to 40% of shoulder dystocia cases, according to Advanced Life Support in Obstetrics (ALSO), a training program for maternity healthcare providers.
- P – Suprapubic Pressure
While the delivering obstetrician applies gentle downward traction to the child’s head, an assistant is advised to push down above the mother’s pubis. Ideally, pressure will be applied for between 30 to 60 seconds, directly over the child’s shoulder, in a rhythmic pattern. Suprapubic pressure is meant to gently coax the fetus into drawing the stuck shoulder closer to its body, thus allowing the entire body to pass under the pubic bone.
- E – Enter
If external remedies have little effect, obstetricians are advised to attempt internal maneuvers with caution. While several different methods have been described, and at least four remain in common practice, all of these maneuvers are intended to rotate the fetus’ stuck shoulder away from the point of obstruction.
- R – Remove The Posterior Arm
In this technique, the obstetrician inserts his or her hand far into the vagina, attempting to locate the fetus’ unobstructed arm. After finding the arm, the child’s elbow should be bent across its chest. The Advanced Life Support in Obstetrics (ALSO) program advises physicians to grasp the child’s forearm, rather than its upper arm, to avoid breaking the bone. Performed correctly, the child’s arm can be pulled free of the birth canal, rotating the child and freeing its obstructed shoulder. Obstetricians rarely attempt this maneuver until several other strategies have failed to safely deliver a child. For obvious reasons, delivering an infant’s posterior arm presents a significant risk of birth injury.
R – Roll The Mother & Deliver The Posterior Shoulder
In this maneuver, the mother rolls over onto all fours, with her knees under her chest. ALSO considers this “all fours” version of the McRoberts maneuver to be “safe, rapid and effective.” While researchers are still unclear why the technique works, the child’s shoulder often comes dislodged as the mother turns, increasing the size of the pelvic outlet. Gravity is also likely to play a role, along with gentle traction on the child’s head from a competent obstetrician.
With skilled care, many cases of shoulder dystocia can be resolved without an infant sustaining permanent injury. But excessive force and pulling are liable to overextend the brachial plexus nerves running through an infant’s shoulder, potentially leading to lifelong disability.
Can We Prevent Shoulder Dystocia?
Shoulder dystocia is fairly difficult to predict, although researchers have identified a number of risk factors that make the delivery complication more likely to occur:
- Breech deliveries, in which a child enters the birth canal feet-first, often with their arms extended overhead. As the infant progresses through the birth canal, pressures exerted by the vaginal walls and cervix can pinch the arms, leading to brachial plexus damage.
- Maternal health conditions, like diabetes, obesity and uterine fibroids
- Assisted deliveries, in which forceps or vacuum extraction are used to pull a child through the birth canal
- Twin or multiple pregnancies
- Fetal macrosomia, in which a child is much larger than the average infant
Even with these risk factors in mind, shoulder dystocia is often a surprise to both obstetricians and mothers. Preventative measures, including elective c-sections, are not well-supported by the medical literature. Researchers at Brown and Columbia Universities have estimated that, for cases of fetal macrosomia, 3,695 emergency c-sections would need to be performed to prevent one permanent brachial plexus injury.
How Are Brachial Plexus Injuries Treated?
Nearly 50% of brachial plexus injuries resolve of their own accord, many without any medical intervention. Even among those children who require treatment, many will be able to regain near-normal motor function in their affected arm. Physical therapy is often recommended, to strengthen muscles that would go unexercised otherwise and increase range of motion.
In severe cases, pediatricians will recommend a surgical operation. Surgeries for a brachial plexus injury generally have two goals: remove scar tissue that has built up around the injured nerve and, in the event that removing scar tissue is not sufficient to improve nerve function, replacing the damaged nerve with a donor nerve. When a nerve graft is required, the most common procedure removes a healthy nerve from the child’s calf and grafts it to replace the section of injured nerve in the brachial plexus.