Kernicterus is an extreme form of jaundice, the common newborn condition that turns a baby yellow. While jaundice usually goes away on its own, kernicterus can cause permanent brain damage, along with severe neurological disorders.
- Mismanaged pediatric care
- Cerebral palsy lawsuits
Most cases of kernicterus are the result of medical negligence. Your family may be entitled to financial compensation. Contact our attorneys now for a free consultation.
When a child develops kernicterus, it’s almost always medical malpractice.
"Professional & Courteous" Hiring Laurence was the best decision of my life.
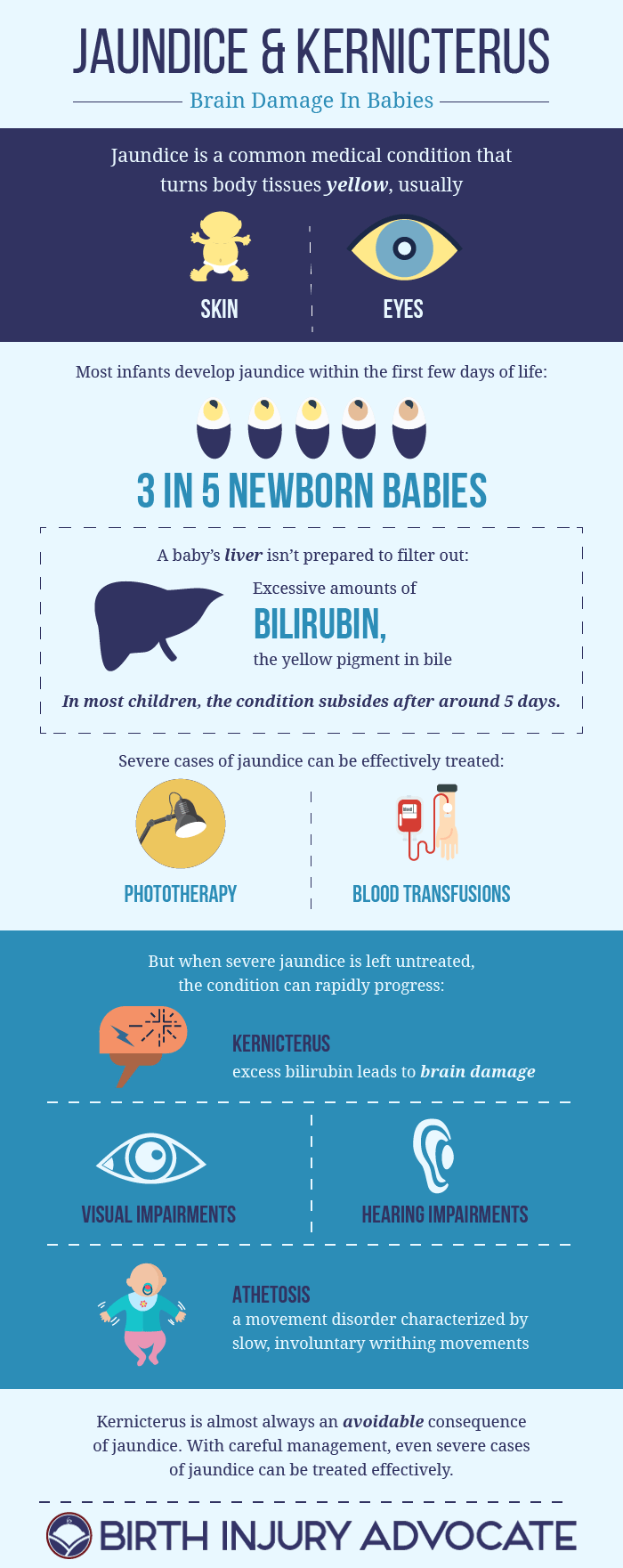
Jaundice is a medical condition, common in infants, in which the skin, eyes and other body tissues turn yellow. While the effects of jaundice can be startling at first, the condition is thoroughly treatable in newborns. When left untreated, on the other hand, jaundice can progress to become a severe neonatal disorder, even causing brain injuries in young children.
Want to share our infographic on your own site? Just copy and paste the code below:
What Is Jaundice?
The term “jaundice” technically refers to the yellow appearance of a child with hyperbilirubinemia, an excessive amount of the bile pigment bilirubin. Bilirubin is yellow, and in infants with jaundice, the child’s skin and eyes can become yellow or orange.
Hyperbilirubinemia
When the body breaks down old blood cells that have become unnecessary, a yellow compound called bilirubin is produced as a byproduct. Healthy children and adults produce bilirubin all the time, but we excrete the compound in our bile and urine – in large part because we have fully-developed livers.
Old red blood cells are initially broken down in the spleen, according to PathologyStudent.com. After that, the bilirubin created as a side effect of this process is passed over to the liver. The liver takes all of this excess bilirubin and pairs it with an acid molecule, which makes the bilirubin “conjugated,” or water soluble. With this final step complete, the conjugated bilirubin can be sent to the small intestine, as a major component of bile, or passed in our urine.
What Causes Jaundice?
Infants, however, aren’t born with fully-functioning livers. Some newborns are unable to filter out enough bilirubin. Instead, the pigment builds up in the blood, turning an infant’s body tissues yellow. The visual effects of jaundice can be harder to notice in babies with darker skin colors.
Jaundice usually becomes apparent during the first few days of a child’s life, and begins to subside around the fifth day. In most cases, a child’s coloration will peak around day three or four, the US National Library of Medicine says.
Mild cases of jaundice go away of their own accord, while more severe cases can be effectively treated if diagnosed appropriately.
Other Types Of Jaundice
While jaundice normally happens because newborn babies can’t process bilirubin well yet, infants can develop the condition for other reasons:
- Poor breastfeeding. In “breastfeeding failure jaundice,” a baby’s inability to breastfeed sufficiently leads to dehydration. The infant urinates less often than normal, which results in a buildup of bilirubin. Breastfeeding failure jaundice is most common in babies born between weeks 34 and 36 of pregnancy. Premature infants often lack the strength and body coordination to breastfeed properly.
- Factors in breastmilk. “Breastmilk jaundice” can run in families. Researchers believe that some chemicals in a mother’s breastmilk can interfere with a baby’s liver function, impairing the organ’s ability to break down bilirubin. This form of jaundice affects around 1 out of every 50 breastfed babies, and can last up to 12 weeks.
- Inadequate liver function. Some babies are born with liver problems, often caused by an infection.
- Rh disease. In a condition called Rh incompatibility, some of a baby’s blood leaks into a mother’s bloodstream during pregnancy. This can cause an increase in the production of white blood cells, which in turn attack the red blood cells of the fetus. Some babies born with Rh disease will develop jaundice.
Jaundice is extremely common. Around 6 out of every 10 babies will develop jaundice after birth, the University of Rochester, with an even higher incidence in pre-term infants and children who developed bruising during labor or delivery.
How To Treat Jaundice
Most newborns with jaundice don’t require treatment. Within two or three weeks, mild cases of the condition should disappear on their own. To treat moderate and severe cases of jaundice, doctors frequently rely on three treatment methods, all of which are intended to reduce the amount of bilirubin in a child’s blood:
- Phototherapy. In light (or “photo”) therapy, newborns are placed underneath a special light that gives off only light in the blue-green range of the electromagnetic spectrum (wavelengths between around 475 and 510 nanometers). These wavelengths of light alter the shape of bilirubin molecules, making them easier to excrete in urine and stool. Doctors take care to filter out ultraviolet wavelengths, which can be harmful, by using a special screen.
- Intravenous immunoglobulin. To treat cases of jaundice caused by Rh incompability, doctors can give babies an intravenous transfusion of immunoglobulin – a protein that lowers the number of foreign antibodies in a child’s bloodstream.
- Blood exchange. In rare cases that do not respond to less-extreme treatments, some infants will require a blood transfusion. Doctors will remove small amounts of a child’s blood, and replace it with blood that has a normal amount of bilirubin. Most newborns require repeated transfusions.
Both jaundice and phototherapy can lead to dehydration. Doctors at the Mayo Clinic recommend that mothers feed babies with jaundice more frequently, supplementing breastmilk with pumped breastmilk or formula if necessary. More frequent feedings can also increase a child’s bowel movements, which may help them pass more bilirubin in their stool.
What Happens If Jaundice Is Not Treated?
Severe cases of jaundice should not be ignored.
While most doctors will diagnose the condition based on an infant’s appearance, the vast majority of physicians will also conduct blood tests to diagnose particularly extreme forms of hyperbilirubinemia.
Visual examination can be misleading; the degree of a child’s coloration is not a good indicator of how much bilirubin has built up in the blood. A skin test is also available; sending a special form of light through a baby’s skin, doctors can measure the light’s reflection and estimate the amount of bilirubin in the blood.
Jaundice should be closely monitored, especially within the first 24 hours of the condition’s appearance. Left untreated, serious cases of jaundice can lead to brain damage in infants.
What Is Kernicterus In Newborn Infants?
Bilirubin is highly neurotoxic, and untreated elevations in the bile pigment can buildup in the brain’s gray matter. In some cases, this buildup will lead to permanent neurological damage. The type of brain damage caused by elevated levels of bilirubin is called kernicterus.
Kernicterus affects the brain in very specific ways, although the condition’s long-term effects will depend on how much bilirubin an infant’s brain has been exposed to. Kernicterus can lead to a wide range of neurological disorders, from minor learning disabilities to athetoid cerebral palsy.
Are Pediatricians Paying Attention?
The severity of jaundice and kernicterus have been downplayed for decades, both among the public and within the medical community.
In 2009, a team of doctors from Stanford and the University of Pennsylvania explained that the “breakdown in systems for safe newborn health-care delivery accounts for the majority of kernicterus cases encountered in the United States.” Writing in the Journal of Perinatology, the group wrote that pediatricians just weren’t following the accepted guidelines for treating jaundice in newborn babies.
Signs & Symptoms Of Kernicterus
For obvious reasons, the most prominent sign of kernicterus is jaundice, a yellow coloration that begins on the face and then spreads to an infant’s chest, stomach, arms and legs.
The initial signs that jaundice has progressed to the point of possible brain damage include:
- decreased alertness
- poor muscle tone (an infant’s limbs may appear “loose” or “floppy”)
- poor feeding
Of course, these are “non-specific” symptoms, ones that could be caused by a number of different disorders. But as kernicterus progresses, the condition’s symptoms become more troubling:
- increased muscle tone (elevated muscle tension at rest)
- retrocollis – a backward arch of the neck
- opisthotonus – a backward arch of the back
- high-pitched crying
- spasmodic torticollis – involuntary and painful movements of the neck
- Parinaud’s syndrome – an inability to move the eyes upward
- fever
- seizures
Some of these symptoms will appear shortly after a child’s birth, while others (like abnormalities affecting the eyes) are more likely to emerge over the course of an infant’s first year.
Complications Of Severe Jaundice & Kernicterus
The most common result of chronic bilirubin encephalopathy, or brain damage caused by high levels of bilirubin, are impairments in hearing. Hearing loss can be mild or severe, according to Medscape, but most children will experience deficits in their ability to hear higher frequencies. This can lead to delays in language acquisition and other developmental milestones.
Athetosis is the most common movement disorder in children with kernicterus-related brain injuries. Children will experience slow, involuntary writhing movements, predominantly in the fingers, hands, toes and feet. Chorea are less common, but also possible. These involuntary movements appear jerky, and usually affect the face, shoulders and hips.
Visual impairments can also be pronounced. Cognitive functioning, however, is rarely impaired, although some children are misdiagnosed with cognitive impairments due to their hearing disabilities.
Can Kernicterus Brain Damage Be Prevented?
Yes.
Kernicterus is almost always an avoidable consequence of jaundice. With proper detection, and careful management, even severe cases of jaundice can be prevented from progressing to kernicterus, the US Centers for Disease Control & Prevention reports. In fact, kernicterus is something doctors refer to as a “never event,” in that it should never happen.
As such, the development of kernicterus in an infant is usually the result of medical negligence.
Once brain damage has occurred, the effects of kernicterus are likely to be permanent. While treatments like physical therapy and speech therapy can help many children improve their motor and auditory abilities, the focus of doctors should be on preventing kernicterus entirely.



